Foods to Avoid with Hemorrhoids: Complete Guide to Dietary Relief
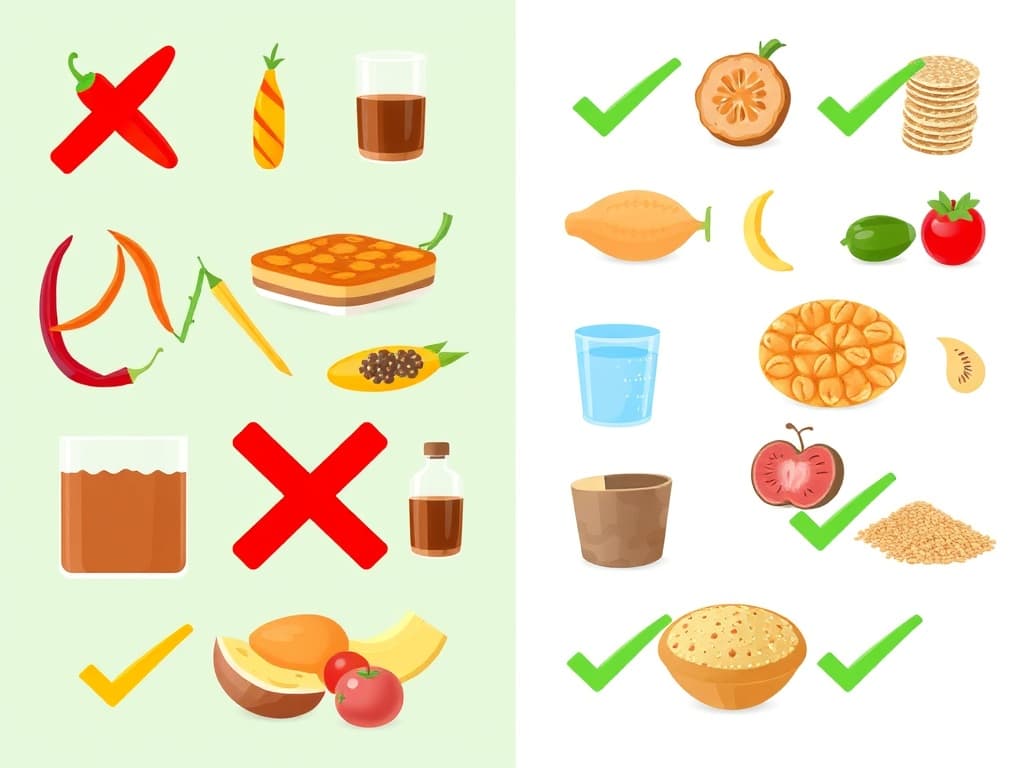
When dealing with hemorrhoids, certain foods can make your symptoms significantly worse. The foods to avoid with hemorrhoids include spicy foods (like chili peppers and hot sauces), processed foods (fast food, packaged snacks), alcohol, caffeine, fried and fatty foods, low-fiber refined grains, high-fat dairy products, and red meat. These foods either cause constipation, dehydration, or direct irritation to hemorrhoidal tissue. By eliminating or reducing these trigger foods and focusing on high-fiber alternatives, adequate hydration, and gentle-on-the-digestive-system options, you can significantly reduce hemorrhoid flare-ups and promote faster healing.
Understanding How Diet Affects Hemorrhoids
Hemorrhoids are swollen blood vessels in your rectum and anus that can cause pain, itching, and bleeding. While many factors contribute to hemorrhoid development, diet plays a crucial role in both triggering symptoms and managing them effectively. The foods you eat directly impact your bowel movements, stool consistency, and overall digestive health. Some foods promote smooth, easy bowel movements that don’t strain hemorrhoidal tissue, while others create harder stools, increase inflammation, or directly irritate sensitive areas. Understanding which foods worsen hemorrhoid symptoms empowers you to make better choices and potentially avoid painful flare-ups altogether.
Spicy Foods: The Heat That Hurts
Why Spicy Foods Aggravate Hemorrhoids
Spicy foods contain capsaicin, the compound responsible for that burning sensation in your mouth. Unfortunately, this same compound doesn’t lose its potency as it travels through your digestive system. When capsaicin reaches your rectum during bowel movements, it can cause intense burning and irritation around already sensitive hemorrhoidal tissue. The irritation isn’t just temporary either. Spicy foods can trigger inflammatory responses that make existing hemorrhoids more painful and swollen. Many people report that their hemorrhoid symptoms flare up for days after consuming particularly spicy meals.
Common Spicy Foods to Limit
The most problematic spicy foods include hot peppers of all varieties, from jalapeños to habaneros. Hot sauces, especially those with high capsaicin content, should be avoided during active hemorrhoid episodes. Spicy ethnic cuisines like authentic Indian curries, Thai dishes, and Mexican foods with heavy pepper use can all trigger symptoms. Even seemingly mild spices like black pepper, when used heavily, can contribute to irritation. During hemorrhoid flare-ups, it’s best to stick with gentler seasonings like herbs, mild spices, and salt-free seasonings.
Processed Foods: The Fiber-Free Culprits
The Problem with Processed Foods
Processed foods represent one of the biggest dietary obstacles for hemorrhoid sufferers. These foods undergo extensive manufacturing that strips away natural fiber while adding unhealthy fats, excessive sodium, and artificial preservatives. The lack of fiber in processed foods directly contributes to constipation, forcing you to strain during bowel movements. This straining puts pressure on hemorrhoidal veins, causing them to swell and become more painful. Additionally, the high sodium content in many processed foods can lead to dehydration, further hardening stools.
Processed Foods to Avoid
Fast food meals are particularly problematic because they’re typically high in fat, low in fiber, and loaded with sodium. Think burgers, fries, pizza, and fried chicken – all delicious but terrible for hemorrhoid management. Packaged snacks like chips, crackers, and cookies offer little nutritional value and virtually no fiber. Processed meats including hot dogs, deli meats, and sausages are not only low in fiber but also high in sodium and preservatives that can worsen inflammation. Even seemingly innocent convenience foods like instant noodles, frozen dinners, and canned soups often contain excessive sodium and lack the fiber necessary for healthy digestion.
Alcohol: The Dehydrating Drink
How Alcohol Worsens Hemorrhoid Symptoms
Alcohol acts as a diuretic, meaning it causes your body to lose more fluid than you’re taking in. This dehydration effect makes your stools harder and more difficult to pass, increasing the likelihood of straining during bowel movements. Beyond dehydration, alcohol can dilate blood vessels throughout your body, including the already swollen vessels in hemorrhoids. This dilation can make hemorrhoids more prominent and painful. Alcohol also interferes with your body’s natural healing processes, potentially slowing recovery from hemorrhoid episodes.
Managing Alcohol Consumption
During active hemorrhoid flare-ups, it’s best to avoid alcohol completely. If you choose to drink occasionally, limit yourself to one drink and follow it with plenty of water. For every alcoholic beverage you consume, try to drink at least two glasses of water to counteract the dehydrating effects. Beer and wine tend to be less problematic than hard liquor, but all alcoholic beverages can contribute to dehydration and symptom worsening.
Need to create a digital menu?
Caffeine: The Double-Edged Stimulant
Why Caffeine Can Be Problematic
Caffeine presents a complex challenge for hemorrhoid sufferers. While it can stimulate bowel movements, which might seem helpful for constipation, it also acts as a diuretic that contributes to dehydration. The stimulating effect of caffeine can sometimes cause urgent bowel movements, leading to straining or incomplete evacuation. This urgency often results in spending more time on the toilet, which puts additional pressure on hemorrhoidal veins. For some people, caffeine also increases anxiety and tension, which can translate to physical tension during bowel movements, making them less comfortable and more likely to cause strain.
Common Caffeinated Products to Limit
Coffee is the most obvious source of caffeine, especially strong brews like espresso. However, don’t overlook other sources like black tea, green tea, energy drinks, and caffeinated sodas. Chocolate also contains caffeine, though in smaller amounts. Energy drinks are particularly problematic because they often contain extremely high levels of caffeine plus other stimulants. If you’re a regular coffee drinker, don’t quit cold turkey as this can cause withdrawal symptoms. Instead, gradually reduce your intake and increase water consumption to maintain hydration.
Fried and Fatty Foods: Slow Digestion Triggers
The Impact of High-Fat Foods
Fried and fatty foods slow down your digestive system significantly. When food moves slowly through your intestines, more water gets absorbed from the stool, making it harder and more difficult to pass. This creates the perfect conditions for constipation and straining. High-fat foods also require more energy to digest, potentially causing inflammation in your digestive tract. This inflammation can extend to hemorrhoidal tissue, making existing symptoms worse. Greasy foods can also cause digestive upset, leading to irregular bowel movements that alternate between constipation and loose stools, both of which can irritate hemorrhoids.
Fried Foods to Minimize
Deep-fried restaurant foods are the worst offenders. French fries, fried chicken, donuts, and other deep-fried items contain trans fats and excessive amounts of unhealthy oils. Fatty cuts of meat like ribeye steaks, pork belly, and lamb chops can also slow digestion. Even cooking methods matter – foods cooked in heavy oils or butter are more likely to cause problems than those that are grilled, baked, or steamed.
Low-Fiber Foods: The Constipation Creators
Understanding the Fiber Connection
Fiber is absolutely crucial for hemorrhoid management because it helps create soft, bulky stools that pass easily without straining. When you eat foods low in fiber, your stools become small, hard, and difficult to eliminate. Refined grains have been stripped of their natural fiber content during processing. This means that foods made from white flour, white rice, and other refined grains contribute very little to healthy bowel movements while taking up space in your diet that could be filled with high-fiber alternatives.
Low-Fiber Foods to Replace
White bread, white pasta, white rice, and products made from refined flour should be replaced with whole grain alternatives. Regular pasta should be swapped for whole wheat pasta, white bread for whole grain bread, and white rice for brown rice or quinoa. Processed breakfast cereals, especially those that are sweetened, typically contain very little fiber. Even cereals that seem healthy can be surprisingly low in fiber, so always check nutrition labels. Baked goods like cakes, cookies, and pastries made with refined flour offer virtually no fiber while being high in sugar and unhealthy fats.
Dairy Products: Individual Sensitivities Matter
When Dairy Becomes Problematic
Dairy products affect people differently when it comes to hemorrhoids. High-fat dairy products like whole milk, full-fat cheese, and ice cream can slow digestion and contribute to constipation in some individuals. Lactose intolerance adds another layer of complexity. People who can’t properly digest lactose may experience digestive upset, irregular bowel movements, or alternating constipation and diarrhea – all of which can aggravate hemorrhoids. The high fat content in many dairy products requires significant digestive energy and can slow the movement of food through your intestines, potentially leading to harder stools.
Dairy Products That May Worsen Symptoms
Whole milk and full-fat yogurt can be problematic for some people, though others tolerate them fine. Hard cheeses like cheddar, swiss, and parmesan are particularly high in fat and low in fiber. Ice cream combines multiple hemorrhoid triggers: high fat content, refined sugars, and often artificial additives. Cream-based sauces and dishes also pack a lot of fat without providing beneficial fiber. If you suspect dairy is worsening your symptoms, try eliminating it for a few weeks to see if your hemorrhoids improve.
Red Meat: The Fiber-Free Protein
Why Red Meat Can Be Challenging
Red meat contains zero fiber while being relatively difficult to digest compared to other protein sources. When red meat makes up a large portion of your diet, it can contribute to constipation simply because it’s taking the place of higher-fiber foods. Red meat also tends to be high in fat, especially cuts like ribs, steak with marbling, and ground beef with higher fat percentages. This combination of no fiber and high fat content creates ideal conditions for digestive slowdown. Some studies suggest that excessive red meat consumption may contribute to inflammation throughout the body, potentially affecting hemorrhoidal tissue as well.
Better Protein Alternatives
Lean poultry like chicken breast and turkey provide protein without excessive fat. Fish and seafood are excellent alternatives that often contain beneficial omega-3 fatty acids. Plant-based protein sources like beans, lentils, and quinoa offer the double benefit of protein plus significant fiber content. These foods actively help with hemorrhoid management while meeting your protein needs. If you do eat red meat, choose leaner cuts and pair them with high-fiber vegetables and whole grains to promote better digestion.
What to Eat Instead: Hemorrhoid-Friendly Alternatives
High-Fiber Food Recommendations
Focus on whole grains like oats, quinoa, brown rice, and whole wheat products. These provide the fiber necessary for soft, easy-to-pass stools. Fresh fruits and vegetables should make up a large portion of your diet. Apples, pears, berries, broccoli, Brussels sprouts, and leafy greens are all excellent sources of fiber and nutrients. Legumes including beans, lentils, and chickpeas are fiber powerhouses that also provide protein and important minerals.
Hydration and Fluid Intake
Water is your best friend when managing hemorrhoids. Aim for at least 8 glasses per day, and more if you’re active or live in a hot climate. Herbal teas can contribute to fluid intake while providing soothing benefits. Chamomile and ginger teas are particularly gentle on the digestive system. Avoid counting caffeinated or alcoholic beverages toward your fluid goals, as these can contribute to dehydration.
Creating Your Hemorrhoid-Friendly Meal Plan
Daily Dietary Guidelines
Aim for 25-35 grams of fiber per day, but increase gradually to avoid digestive upset. Start by adding one high-fiber food per day and slowly build up your intake. Eat regular meals rather than skipping meals or eating large portions infrequently. Consistent eating patterns help regulate bowel movements. Include a variety of colors in your fruits and vegetables to ensure you’re getting diverse nutrients that support overall digestive health.
Sample Menu Ideas
For breakfast, try oatmeal with berries and a small amount of nuts, or whole grain toast with avocado. These provide fiber and healthy fats without being heavy on your digestive system. Lunch might include a large salad with mixed vegetables, beans, and lean protein, or a soup made with vegetables and legumes. Dinner could feature grilled fish or chicken with steamed vegetables and quinoa, providing protein, fiber, and essential nutrients without foods that trigger symptoms.
When to Seek Professional Help
Consulting Healthcare Providers
If dietary changes don’t provide relief within a few weeks, consult your healthcare provider. Persistent or severe hemorrhoid symptoms may require medical intervention beyond dietary modifications. Some people benefit from working with registered dietitians who can create personalized meal plans based on individual triggers and preferences. Don’t ignore severe symptoms like excessive bleeding, intense pain, or hemorrhoids that don’t respond to conservative treatment.
Personalized Nutrition Recommendations
Everyone’s digestive system responds differently to foods. What triggers one person’s hemorrhoids might be perfectly fine for another person. Keep a food diary to identify your personal trigger foods. Note what you eat and any symptoms that follow, looking for patterns over time. Work with healthcare professionals to develop a sustainable long-term eating plan that supports both hemorrhoid management and overall health.
Conclusion
Managing hemorrhoids through diet requires avoiding foods that contribute to constipation, dehydration, and direct irritation. By eliminating or reducing spicy foods, processed foods, alcohol, excessive caffeine, fried foods, low-fiber refined grains, high-fat dairy, and red meat, you can significantly reduce hemorrhoid symptoms. Remember that dietary changes work best when combined with other healthy habits like staying hydrated, getting regular exercise, and not delaying bowel movements when you feel the urge. The key is finding an approach that works for your individual needs while ensuring you still enjoy your meals. With patience and consistency, dietary modifications can provide substantial relief from hemorrhoid symptoms and help prevent future flare-ups.
Frequently Asked Questions
Can I eat eggs if I have hemorrhoids? Eggs are generally fine for hemorrhoid sufferers as they’re easy to digest and don’t typically cause constipation. However, pair them with high-fiber foods like vegetables or whole grain toast for optimal digestive health. Are bananas good for hemorrhoids? Yes, bananas are excellent for hemorrhoids because they’re high in fiber, easy to digest, and contain potassium which supports overall digestive health. Ripe bananas are particularly beneficial. What should I drink with hemorrhoids? Water is the best choice, along with herbal teas and diluted fruit juices. Avoid alcohol, excessive caffeine, and carbonated beverages which can worsen symptoms. Can chocolate worsen hemorrhoids? Chocolate can potentially worsen hemorrhoids because it contains caffeine and is often low in fiber. Dark chocolate in moderation is better than milk chocolate, but it’s best to limit chocolate during flare-ups. How long does it take for dietary changes to help hemorrhoids? Most people notice improvements within 1-2 weeks of making dietary changes, though it can take up to a month to see significant results. Consistency is key for lasting relief. Should I avoid all dairy with hemorrhoids? Not necessarily. Low-fat dairy products like yogurt with probiotics can actually be beneficial. However, high-fat dairy products like whole milk and cheese may worsen symptoms in some people.
